A new mental health collaborative was inspired to come together after the Health Partnership Symposium, Petty and Randy explain why sharing knowledge and practice across country borders is so crucial in the battle to improve mental health care.
“Seeing
mental health and substance misuse patients suffering, neglected by the
community, families and other healthcare workers; motivated me to work with
mental health. Working as a health Administrator and a Project Coordinator at a
Tanzania National Mental Health Hospital, I found I could help these
individuals so that they can be provided with an environment that will allow
them to recover from their illnesses, reduce relapses and lead a normal life.”
Perpetua
Mwambingu- Tanzania Link Project Coordinator
“In
Ghana mental illness is often attributed to spiritual causes and people who
suffer from mental illness do not get the help that they need. Stigma and
discrimination is high and people who suffer from mental illness lose their
dignity, respect and self-worth. My passion for awareness creation and advocacy
and my belief that someday Ghana will appreciate the importance of mental
health motivates me even during moments of burnout”
Randy Agbodo- Project Lead for Ghana - Zambia - NHS Highlands Partnership
The Story
Remains the Same
According to the
World Health Organization, for every four people, one will be affected by a
mental or neurological disorder in their lifetime. The magnitude of mental
health burden is not matched by the size and effectiveness of the response it
demands. Currently, more than 33% of countries allocate less than 1% of their
total health budget to mental health[1].
Sadly, in
Tanzania and Ghana where Randy and I are working, the story remains the same,
mental health services are underfunded, and most of the donor funded programs
go to communicable diseases. There is inadequate human resource and
insufficient supply of medications. Stigma and discrimination towards persons
with mental disorders is still prominent and effective mental health prevention
and promotion programs are woefully inadequate.
No Health without Mental Health
Depression is
ranked first in the list of top ten leading causes of years lived with
disability (YLDs)[2].
Globally, an estimated 350 million people of all ages suffer from depression[3].
At its worst depression can lead to suicide and close to 800,000 people die due
to suicide every year[4].
This is why it
is so vital that World Health Day this year is addressing depression, bringing it
to the fore of global health discussions. It gives health managers and policy
advisers the opportunity to appreciate that depression affects productivity and
therefore prioritizing and investing heavily in mental health would, in the
long run, culminate in populations with healthy outcomes, respect for human
rights and stronger economies.
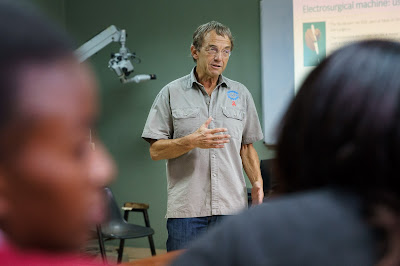
The Health
Partnership Symposium ‘effect’
In order to make
this a reality, we believe that collaboration and the sharing of approaches is
key and at the recent Health Partnership Symposium, organized by THET, we found
we were not alone in this thinking.
Our passion for
working in mental health was further cemented at the event where a certain
chemistry brought colleagues from Ghana, India, Kenya, Nepal, Scotland,
Tanzania, Uganda and Zambia together to form the ‘Mental Health group’.
We all wanted to
come together to tackle and develop our learning on different mental health
issues. Ultimately we wanted LMIC’s to
start collaborating and to share experiences which can strengthen the
partnerships we work in. That’s when a luncheon ‘chat’ was called, then a
dinner ‘talk’ happened and then we came to form a WhatsApp group, a way for us
to easily reach out to each other.
The world is
facing many challenges; political unrest, war, economic hardship, unemployment,
etc., all are contributing factors to depression. This must be a wake-up call
for the global community, the need to re-think, and re-act to this global
crises, now is the time to re-set our priorities with regards to mental health
and to act together through partnerships and shared learning. After all there
is no health without mental health.
Perpetua
Mwambingu
Tanzania Link Project
Coordinator,
Tanzania
Randy Agbodo
Project
Lead for Ghana - Zambia - NHS Highlands Partnership,
Ghana