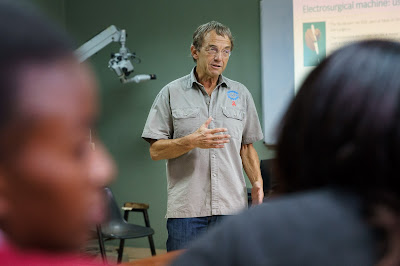
On Day 1 of THET Annual Conference 2016, ‘Evidence, Effectiveness & Impact’, Lawrence Loh chaired the breakout session entitled ‘Network for collaboration: partnership communities and volunteers contributions’. Here the highlights of the session.
I recently had the pleasure of
attending the 2016 Tropical Health and Education Trust conference held 20-21
October at Resource for London and chairing the breakout session titled “Networks
for collaboration: partnership communities and volunteer contributions.”
In keeping with the conference
theme of Evidence, Effectiveness and Impact and focus on health partnerships,
the presented valuable abstracts covered the full range of tools and
topics around partnerships. These included tools to measure and visualise
partnerships and networks; frameworks to assess a partnership or coalition’s
development phase; strategies to tangibly measure the outcomes of partnerships;
and of course, broad descriptions of how partnerships might better support
sustainable, positive development impacts on communities worldwide.
The first presentation, from
Kristy Yiu of McMaster University, reviewed the results of a network mapping
analysis conducted on a novel community health partnership in the Dominican
Republic. The specific aim of this coalition is to bring visiting short-term
volunteer groups into the fold of established development efforts identified by
the communities, thus eliminating the “parallel system” of programming created
by foreign visitors. To move the partnership forward, Yiu and her co-authors
analysed the range of connections between coalition partners and evaluated
their perceptions around the coalition’s strengths and weaknesses. By doing so,
Yiu’s work aimed to show the value of network analysis in planning and
developing global health partnerships.
Dr. Oliver Johnson of Africa
Health Placements (AHP) then shared a summary of post-experience survey evaluations
from their participants. The studied population was largely junior doctors
placed by AHP in Africa based rural hospitals for year-long placements to
support health human resource gaps. In doing so, African-based partners were
described as having a notable role in leading the recruitment and assignments
in question. The surveys found that partnerships with a local facility meant
greater engagement between parties, and interestingly, a commitment from
participant junior doctors to undertake quality improvement projects while on
the ground there – perhaps reflective of an unintended shift in volunteer
mindset towards capacity building rather than strict service provision.
The next talk from Dr. Katie
Mageean also emerged from an African project that focused on the evaluation
results arising from a partnership-led paediatric triage intervention in
Uganda. Dr. Mageean’s work helped demonstrate the substantive outcome of health
partnerships. In her specific example, local partner leadership and buy-in was
essential to facilitating training and support for local staff, which in turn
supported the success of the intervention in changing process outcomes. Her
presentation closed by highlighting additional ongoing research work that is
targeted at documenting improved patient outcomes from this capacity building
partnership effort.
The last and final presentation
by Dr. Annalee Yassi presented a “North-South-South” partnership model based on
the development of partnerships between a Canadian institution and its South
African counterpart. In this specific model, technical expertise around health
challenges was sought through an initial international partnership
(North-South) that then was distributed through a national network of peers
(South-South). Dr. Yassi shared lessons learned and opportunities that such a
model might provide, highlighting the need for a strong, respected southern
partner to act as the key modulator between the two relationships and bring
information and identified needs from their South-South “community of practice”
as part of the conversation within the North-South partnership. In turn, that
same partner would be expected to bring and disseminate international inputs
within the South-South partnership.
The session ended with a panel discussion
featuring the presenters that drew out common themes among their work.
Questions focused on tools to understand and measure the outcomes of
partnerships to show their value, and the importance of flexibility in
developing and tweaking differing partnership models depending on context and
priorities. The perspective of trust and openness from local partners was also
highlighted as one potential area to explore that had not been touched on.
In all, the session was extremely
fruitful and provided a lot of food for thought around how we understand and
evaluate the nature of health partnerships in global health work. As with all
good sessions, many left with more ideas and questions than they started with!
Lawrence C. Loh, MD, MPH, CCFP,
FRCPC, FACPM
See pages 23-26 of the Abstract Booklet for more information about the work of
the partnerships featured in this blog.
I recently had the pleasure of attending the 2016 Tropical Health and Education Trust conference held 20-21 October at Resource for London and chairing the breakout session titled “Networks for collaboration: partnership communities and volunteer contributions.”